 By Richard A. Lewis, M.D., M.S.
By Richard A. Lewis, M.D., M.S.
Many different disorders of the eye affect the stability of the tear film; an unstable tear film is a hallmark of “dry eyes”. Proper classification of the cause of a tear deficiency is critical for several reasons:
- Appropriate therapy depends on proper diagnosis;
- Certain conditions of dry eyes are associated with sight-threatening complications in the cornea (the transparent “watch crystal” of the front surface of the eye); and
- Some conditions are associated with systemic immune abnormalities that may affect other organ systems.
In general, dry eyes can be categorized into two major groups, those in which there is inadequate production of the watery component of tears, and those in which the volume of water seems to be normal. However, since water alone is not the only component of tears, other aberrations in both the oil component and the mucous component can be defective and lead to the same symptoms of inadequate lubrication and moistening.
Deficient Watery Tear Production
Inadequate production of the water component of tears is produced by an under secreting tear gland, reducing the amount of tear production and tear flow. Sometimes called keratoconjuctivitis sicca (KCS), there is drying of both the surface of the cornea and the surface of the white part of the eye and inner surface of the lids from inadequate moisture.
Dry Eye with Adequate Watery Tear Production
The other major category of dry eye includes those conditions with adequate watery tears, but abnormal tear dynamics as a result of increased tear evaporation. One cause is an abnormal function of the oil glands in the eyelids that produce the protective oily layer on the outside of the tear film. The normal function of this oil layer is, just as oil on water, to prevent the watery component of tears from evaporating. If there is scarring of the oil glands in the eyelids,the volume of oil is reduced and therefore the tear film is unstable and evaporates more rapidly, leading to the same symptoms as water deficiency.
Therapy of Dry Eye
Currently, the treatment of the irritation associated with dry eyes is largely directed at providing relief of the symptoms. Strategies are aimed at lubricating the surface of the eye and conserving tears that have produced. The mainstay of treatment for decreased aqueous tear production is topically applied lubricants and ointments.
Although these agents often provide temporary relief of the symptoms, they obviously do not reverse the abnormalities of the ocular surface when the cells may be lost or scarred, especially over many years. Despite the availability of huge numbers of commercially available artificial teardrops, at the present time none is a true therapeutic tear replacement with normal biological activity.
As a result, some individuals with severe tear deficiency and severe ocular irritation must put their artificial teardrops in several times an hour to keep their symptoms tolerable.
Preservative-free artificial tears should be considered by anyone who feels that they must instill these medications more than four or five times a day to relieve and control their symptoms. Dozens of such preparations are available “over-the-counter”, without prescription, in any large pharmacy.
Symptomatic individuals are encouraged to buy small bottles of several different brands to find one that is most soothing and that relieves the symptoms.
Lubricant Ointments
Lubricant ointments, which are basically sterile “grease” or “oil” in a solid form, are particularly useful before going to bed, because they have a longer contact time than drops and they will coat the surface of the eye during sleep, when the normal tear production is reduced.
People with very severe dry eye may also use lubricant ointments during the daytime, but most of them are bothered by the blurred vision, the sticky sensation, and “smear” experienced after the ointment that may last 15 to 30 minutes after each application.
Other Interventions
Individuals who continue their symptoms in spite of maximal artificial tear supplements may benefit from other interventions aimed at saving their reduced volume of their inherently produced tears.
A humidified environment is recommended to reduce tear evaporation. Tear evaporation can also be reduced by placement of side panels and moisture chambers around the frames of eyeglasses. Covering the eye at night or even taping the lids closed may also reduce tear evaporation. Some individuals may actually benefit from wearing swim goggles or by taping a plastic shield or plastic wrap over the eyelids at bedtime.
Punctal Occlusion
One of the most useful and practical therapies from conserving tears is punctal occlusion. The punctum is the medical name for the small “drain” near the corner of the eyelids, through which tears drain into channels down into the nose.
Temporary occlusion of the punctum with small collagen plugs, and more recently with permanent plastic or silicone plugs that can be removed, are major advances. Indeed, some of my patients have silicone plugs in place for seven to ten years without any complication.
Permanent punctal occlusion, performed either with a cautery or with a laser, can completely obliterate the lacrimal puncta. Unfortunately, if there is ever a need for reopening the punctum, it cannot be done in any fashion, other than by an extensive surgical reconstruction, once it has been obliterated by these destructive methods. Therefore my bias has always been to use the silicone plugs, which can be removed easily if they are no longer needed.
Dry eyes are a common feature of some of the ectodermal dysplasias, because of abnormal tear glands, lid disease, or defective production of the mucus, the water, or the oil layer of tears. Treatment of dry eyes in these situations is exactly the same as dry eyes in any of these situations.
What Doesn’t Work?
Not infrequently, members of the National Foundation for Ectodermal Dysplasias (NFED) ask about the use of a drug advertised on television for the management of symptomatic “Dry Eyes”, particularly for women in middle age who are approaching menopause. Restasis is the tradename of the topical (eye drop) formulation of cyclosporine. Cyclosporine is an immune suppressant, discovered originally in Japan, and now used by the solid organ transplant teams to modify or prevent organ rejection in such procedures as heart, lung, and kidney transplant patients.
Although advertised heavily on TV and other media for the relief of post-menopausal dry eyes and for management of some autoimmune dry eyes as in rheumatoid arthritis and systemic lupus erythematosus, the use of Restasis in the ectodermal dysplasias makes no logical sense, since the ‘cause’ of the dryness is not immune-mediated but inherent in the genetic origins of the tissues and cells that manufacture the tears and the oils and mucus components of tears. In fact, while Restasis is widely used for this intended “autoimmune” set of disorders, its use is expensive and none of the members of the NFED for whom it has been prescribed has had a beneficial outcome.
Recently, during the 2016 summer, a new drug named Xiidra™ (lifitegrast ophthalmic solution) 5% was approved as the “first new agent in 20 years for dry eyes”. This is a small molecule LFA-1 antagonist mostly in lymphocytes and has an effect on vascular endothelial cells and conjunctival epithelial cells, so this molecule blocks trafficking and retention of the immune cells in the conjunctiva.
Once again, there is no logical expectation that this immune suppressant drug “should” have ANY beneficial effect on the tear deficiency in any of the ectodermal dysplasias. It is too new to have any NFED members comment about both the expense and benefits, but I suspect from its mechanism of action in an immune pathway, that this agent also should offer no benefits. But time and experience will guide future recommendations.
– Dr. Lewis is a Professor in the Departments of Molecular and Human Genetics, Ophthalmology, Medicine, and Pediatrics, Baylor College of Medicine, Houston, Texas. He is a member of the NFED Scientific Advisory Council.
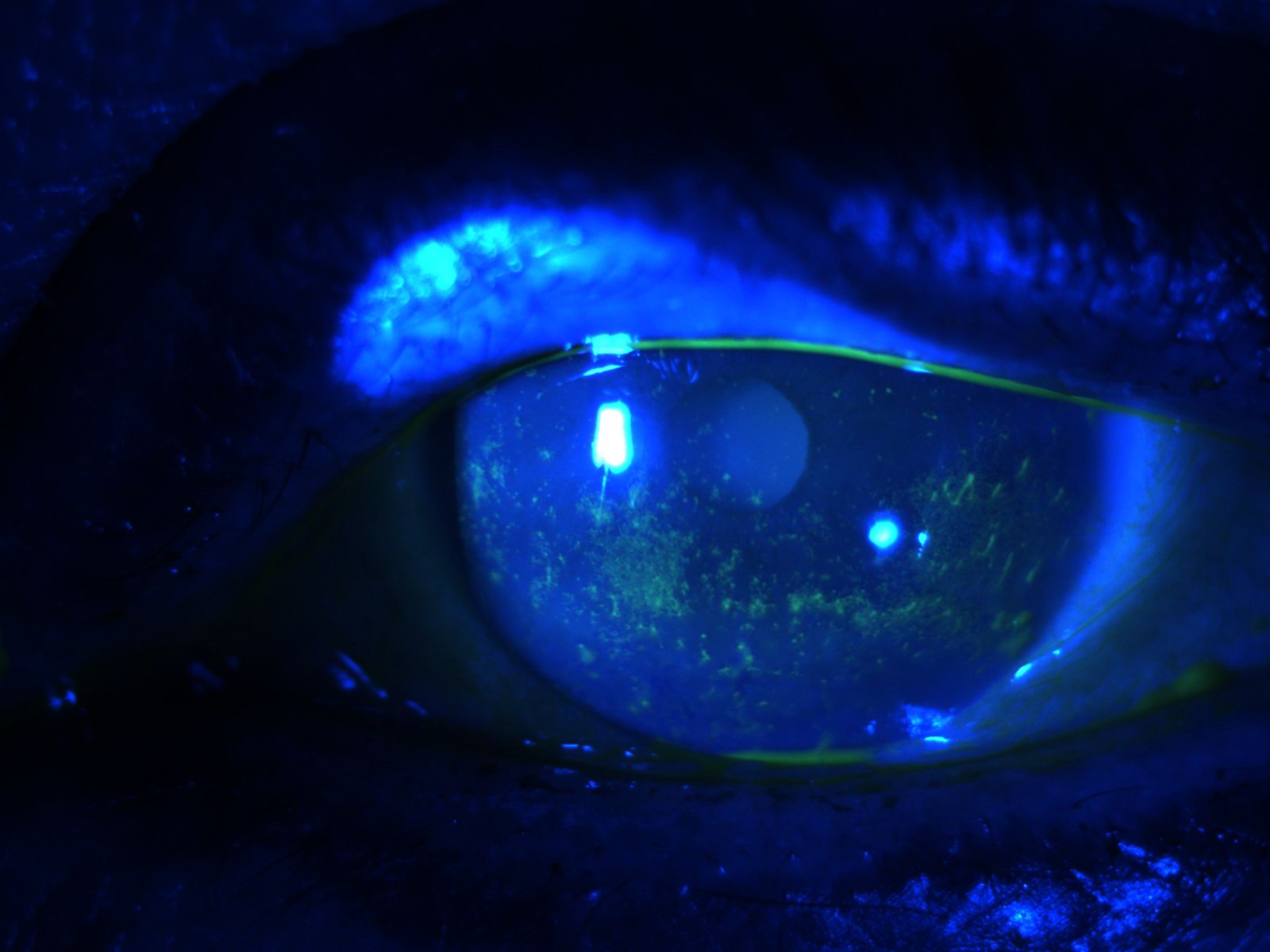
Photo courtesy of Stephen Pflugfelder, M.D., Professor of Ophthalmology, Baylor College of Medicine.
Editor’s Note:
Do you or your loved one affected by affected by ectrodactyly-ectodermal dysplasia-clefting (EEC) syndrome or ankyloblepharon-ectodermal defects-cleft lip and/or palate (AEC) syndrome have dry eyes and/or corneal scarring that persists in spite of aggressive lubrication? We have some information that we would like to share with you that might be helpful. Contact Mary Fete, NFED Executive Director if you are interested.
Other Blogs you may be interested in:
This article was SO helpful, thank you! I have XLHED, and chronic dry eyes. I was prescribed Restasis and took it for a few months, but saw no results other than the discomfort after putting in the drops. But these days I’m desperate, so I was thinking of going back on it. Now I’ll skip that. So thank you!
Yes, indeed, this was very helpful. I too have XLHED and now, over the last 10 years (I’m aged 51) have been battling macular telangiectasia. Is there a connection between HED and this particular macular disorder? Thank you.
Back in 2004 my eyes got very, very bad – inflamed, red, sore, vision loss. I went to many doctors and experience many different tests to determine the cause – why the sudden onset? They ended up putting me on Restasis, and I have seen an improvement. As many of you know, Restasis is very expensive even with insurance. I go to a clinic/pharmacy where I qualify for the 340B program, I it reduced my cost significantly. I encourage everyone to ask their pharmacy about it. The pharmacy that I use is I think state and federally funded. It’s not like going to Kroger, Walmart, Target, CVS or Walgreens. I don’t know if they are able to offer the 340B program or not, you will have to ask. Recently my cornea specialist prescribed Xiidra. I obtained it for FREE by using a card that was provided in a pamphlet distributed by Xiidra. Unfortunately I have only used it once because of the severe burning. I will try it again in the near future.
I have been using Restastis just over a year — I’m still not sure that it helps — it still burns most of the time and it is expensive– I do find the daily warm compresses in the am and pm helpful and they always feel good.. What has helped a lot during a flare up is Lotemax, however you are not supposed to use it for too long or too often from what I understand. I have an appointment in a few weeks to address all with my eye doc. I will follow up with any new news..
good information. My eyes get dry so this is good to know